Electronic Health Record Interoperability
EHR systems have long been associated with healthcare services as a digital file transcript that allows medical records and patient history data to be shared more securely across cross-departments. EHR is committed to relieving the physician of his administrative duties and assisting in obtaining more positive outcomes. Over the years, EHR system users have seen several benefits, including more secure and convenient patient data exchange between rural, urban or large hospitals and ease of patient access to medical records.
EHR interoperability has been the topic of much discussion recently about using the EHR system between the Department of Public Health and the Federal Department of Health Administration. As a result, Healthcare organizations have focused on several innovative initiatives, such as new trends in EHR interaction between healthcare providers in the federal and private sectors and new integrations between different management departments.
What is EHR interoperability?
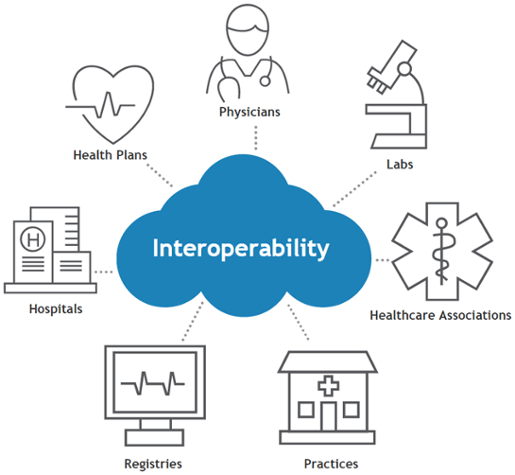
EHR interoperability is a process that allows patient information to be shared electronically to other departments through health care systems. Interoperability has been described as the most important and central concept of an EHR system, but there are different levels of information exchange for a security organization.
By HIMSS definition, interoperability is the ability to coordinate across other information systems and applications and communicate within boundaries of organizations and departments. EHR interoperability is essential in personal access to data, secure exchange of medical records, and access to historical medical records.
EHR interoperability standards in modernization
Small practices face some challenges in sharing medical data and patient history records among the more complex electronic reports. However, other organizations have been making the most of EHR interoperability for some time. The Department of Expertise aims to make it the most advanced and powerful electronic reporting interoperability for ministries worldwide, including mini-practices.
All the plans aim to improve the electronic sharing of sensitive data by eliminating physical communication. However, the recent global development of EHR systems and the fact that more and more companies are systematically organizing interactive plans makes it difficult for the patient to adjust the interface.
Accordingly, there are a number of the latest standards of healthcare interoperability going hand in hand with modernization. Its broadest standard is FHIR (Fast Healthcare interoperability), as well as FHIR, is a mighty effort dedicated to creating the latest and largest community of data sharing. H Level Seven organized FHIR. The Department of Trends sees FHIR as a significant overhaul of interoperability.
Between the Department of Defense and the Department of Public Health, which has existed since 2000. FHIR, a more sophisticated, faster, safer, more interactive process that meets specific standardization requirements, is undergoing upgrades. As a result of improving the patient care process, millions of people worldwide have access to Department of Defense data. FHIR standards are capable of retrieving data more than 60% faster than a typical EHR process.
Over the next few years, the Department of Trends is taking steps to strengthen EHR access further, accelerate to 99% and improve interface connectivity with commercial providers. In addition, with the use of custom software systems over the years, the Department of Trends plans to turn it into a new trend and modernize interoperability. That is the introduction of the use of COTS. Their process of introducing the COTS product is by investing it in interactive tools. The great advantage here is that these products can enter clinical data without interruption.
Importance of modernizing the EHR interoperability process
Whatever the standardization process, it should interact more systematically through pharmacies, other clinics and laboratories. No matter how active EHR systems are worldwide, patient access to clinical data will be limited if physician and nurse access is limited. Modernization is essential to improve the security of information while making communication more efficient.
The purpose of the update is to enable faster access to real-time data for any healthcare worker who needs specific patient data records. Technological modernization of the EHR interactive process is also essential to gather data by navigating through multiple sources and freeing healthcare professionals from propagators.
Healthcare organizations have several separate functions for securely exchanging data, that is, interacting. These include TigerConnect Patient Engagement, CMS and MYHealthEData programs. While these programs are primarily focused on the EHR interaction process, they also contribute to streamlining the communication of healthcare organizations.
Objectives of the EHR in interoperability modernization
The main objectives of modernizing DOD and VA integration are to enhance interoperability in integrating an extensive system network. Accordingly, among the goals is to launch a care plan to manage wellness. Uses of the more integrated EHR systems Cerner and Epic have already increased. Among the interactive objectives, tasks such as scheduling appointments, a systematic review of reports, etc., are another idea to improve with the development of communication.
VA’s primary goal is to further enhance the relationship between federal and other industry partners through the EHR interactive process, with one of the CEOs of the VA Office saying of EHR modernization, “We are developing the best care tool that people need.”
They aim to deploy new software as well as meet the challenges of existing workforce training. It also seeks to save costs by upgrading current EHR systems rather than experiencing software programming delays, activation issues, data access, and transferring specific barriers to other software.
Expanding the modernization of EHR interoperability
The interaction of more data centres should be increased to facilitate communication while enhancing interoperability. VA is already integrating several large database centres around the world. According to a review of the VA Update Policy 2 years ago, 24 of the 375 databases across the United States were covered. And that more would be doubled in the future.
The current EHR interoperability is likely to change rapidly over the next few years against a backdrop of technologically accelerating globalization. Accordingly, the ownership of the EHR interaction between VA and DOD may change over time and with the landscape. The need to include COTS products or commercial (Cerner, Epic) products will continue to grow, and their growth must continue to thrive. VA has also taken steps to deploy FHIR’s data service architecture targeting the landscape. There, they aim to improve the interoperability of HIE’s integrated systems.
VA has also taken steps to launch strategic plans to expand the modernization of EHR interoperability. They have made EHR use easier for beginners and current employees by improving the infrastructure through technology. By VA, to enhance the deployment of EHR systems through the latest research methods, inefficient systems have been eliminated. Taking full advantage of its commercial capabilities, VA has also made the technology of cloud-based applications faster and easier to integrate.
Does the modernization of EHR interoperability help small practices?
Modernization of EHR interoperability is currently being implemented through larger practices. Still, if they want to expand it more effectively worldwide, they will inevitably have to look at smaller conventions. However, it is possible to combine many small practices with the same aim to gain the bargaining power to implement the latest standards, compatibility, technology, and more practical applications required for interoperability.
A single meeting of those small practices can be further expanded and carried forward through exchanging information and communication through interoperability. Over the next few years, HIEs will truly grow exponentially, regionally and statewide, and smaller practices may have the size and protection needed to adapt to change.
Also, as the modernization of interoperability expands rapidly, large companies, sellers, and consultants seek advice for change. Accordingly, the modernization of interoperability, directly and indirectly, affects small practices. In addition, small practices benefit from interoperability, such as the benefits of health care processes and increased patient confidence in compliance.

